| http://www.magnesiumhilfe.de/poster200309.php, version of: September 9, 2006. |
|
Self-Help Organisation Magnesiumhilfe Poster, September 2003 |
|
Poster at the 10th International Magnesium Symposium, September 7-11, 2003, Cairns, Australia About the misdiagnostics of Magnesium deficiencyD.-H. Liebscher (Berlin), D.-E. Liebscher (Potsdam)
Self-Help Organisation Mineral Imbalances |

|
Magnesium deficiency is abundant, but mostly unspecific, due to the general role of Magnesium inside and outside the cell. Hence its diagnostics is open to many errors. |
|
Download: (Various systems may not support all formats.) (Gziped Postscript Format - PS, 260kB) (Portable Document Format - PDF, 173kB) |
|
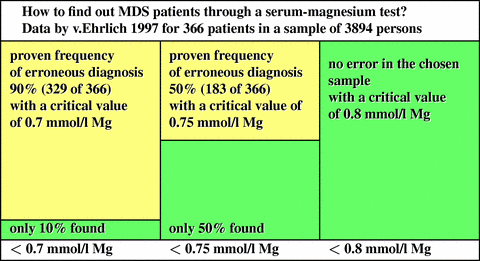
Let us assume that the practitioner has identified the symptoms as part of the magnesium deficiency syndrome and intends to start a test based on the value of the serum concentration of magnesium. In the literature, a host of different critical values are mentioned (0.8 mmol/l Mg [3,4,5], 0.75 mmol/l Mg [6,7,8], 0.7 mmol/l Mg [9,10]), but most of them without correct statistical foundation. We derive from the data published by v.Ehrlich in 1997 [11] that
The estimation of the mean value for the normomagnesiaemic persons without clinical symptoms varies about the value of 0.9 mmol/l Mg. When the distribution for the affected is Gaussian, a critical value of 0.9 mmol/l Mg misses only 1% of the affected. v.Ehrlich had diagnosed 366 (9,4%) patients among 3894 in total which had symptoms belonging to a clinically relevant magnesium deficiency syndrome (MDS) and showed less than 0.8 mmol/l Mg [3,4,5]. When patients with more than only 0,7 mmol/l Mg [9,10] would be considered as normomagnesiaemic, more than 329 magnesium-deficiency patients would be erroneously declared as normomagnesiaemic. In these cases (that cover 90% of the affected patients!) unfortunately, no magnesium therapy would be started. Taking 0,75 mmol/l Mg [6,7,8] as critical value, v.Ehrlich still had missed 183 (50%) of the affected patients. We conclude that 0,8 mmol/l Mg is the critical value to be applied, when not more than 10% of the affected patients shall be missed. When a therapy is started, it should not be reduced before the MDS patient reached the value of 0,9 mmol/l Mg. |
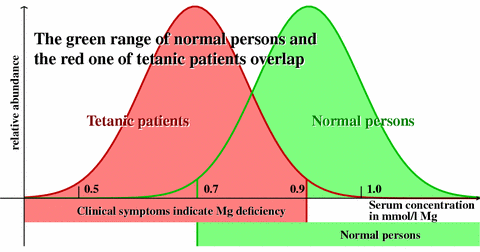
It is a famous error in statistics to use the confidence limits of the normal population as exclusion limits for the affected (see the diagram below). In any decision between two alternatives (here: normal person and patient) two distinct errors are present: First, a person without magnesium deficiency can erroneously be decided to have a deficiency (error of the first kind). Second, a patient with deficiency can erroneously be declared normal and remain undetected (error of the second kind). The decision procedure decides about the value of both errors, and can be chosen to fix one of the two. Usually (because it can be determined by calculation), the error of the first kind is chosen to be 0.05 or 0.01. However, the smaller the error of the first kind is chosen, the larger the error of the second kind will necessarily be [12]. In most cases - and our case belongs to these - the error that implies the higher risk or the higher costs must be made small. In our case, this is the error of the second kind, i.e., the costs of the untreated illness. The decision through use of the serum concentration must respect the distribution of this value for affected patients, and must not use the distribution for normal persons. In 2000, we estimated the distribution of the serum value for affected patients much too conservative. As the data of v.Ehrlich show, the mean value of the left distribution is larger than 0.75 mmol/l Mg, and only 10% of the red area lie left to 0.7 mmol/l Mg. The distribution for the affected patients must be shifted to the right, but could be narrower. The exclusion of a MDS can be safely done only for critical values higher than 0.8 mmol/l Mg. |
|
Magnesium is an essential element occurring naturally in the body and is not a foreign drug normally absent in the body. Hence, it acts causally, and it is almost free of adverse effects. Magnesium therapy must be considered as first choice in the indicated cases. All first-choice use of drugs runs instead into the danger of poisoning the patient and pushing him in a hopeless situation in which the wrong diagnosis always confirms itself. This is to be accounted for in particular in diagnoses of symptoms that are considered to be of mental origin. |
|